
April 15, 2020
COVID-19 UPDATES
Hello Wise Patients! As always, we are so grateful for the opportunity to care for such an invested and conscientious community. Let’s continue supporting one another. We love hearing what content is useful or educational, and encourage you to share this information with any members of your network who could benefit.
In an effort to address our community’s health care needs while reducing face-to-face visits in clinics we are still offering one-time, $75 telemedicine visits for non-established members. If a patient is happy with their care, they can opt to use their payment for the televisit towards their first month’s membership with Dr. Naomi Lee. We encourage any interested parties to reach out if they have questions.
We Want to Hear From You!
Do you have a way that you’ve been keeping busy, active during this time? Let us know and we might feature your activity in next week’s newsletter and can share it with other Wise Patients!
https://forms.gle/EqVw81AnALMPiJgw5
Telemedicine on the forefront of the COVID-19 response
When COVID-19 caused economic shutdowns and mandated social distancing the way we interacted with the world changed, including interactions with the healthcare system. We have always recognized the positive impact of improving patient access and communication with us outside of face-to-face visits. We were fortunate at Wise Patient that telemedicine has been incorporated in our care model for some time now. As you all have experienced, it gives us tools to continue providing great care for our patients at a distance. With the need for social distancing, the rest of the world is also learning the benefit of leveraging technology to bridge the distance between patient and doctor.
On March 30, the Centers for Medicare & Medicaid Services (CMS) issued what it called “an unprecedented array of temporary regulatory waivers and new rules to equip the American healthcare system with maximum flexibility to respond to the 2019 Novel Coronavirus (COVID-19) pandemic”. This allowed for the coverage of 80 additional services provided via audio and video calls. Ray Dorsey, director of the Center for Health and Technology at the University of Rochester Medical Center (Rochester, NY, USA) notes that “there has been something like a ten-fold increase in the last couple of weeks. It’s as big a transformation as any ever before in the history of US health care.” In New York City, 911 dispatchers are dispatching some calls directly to telemedicine. This mirrors what is occurring in many other countries worldwide. Read more here.
We watch with interest to see how telemedicine is incorporated into the delivery of healthcare beyond COVID-19. More than anything, we are grateful to have forged deep relationships with our patients during our in clinic time so that when we communicate with you via chat, phone or video, we have the context necessary to provide personalized, patient-centered care.
More Connections, More Infections
Amidst our extended period of social distancing, University of Washington professors Dr. Steven Goodreau and Dr. Martina Morris explored the question likely tempting us all: “Can’t I please visit just one friend?” Their recently published study illustrates the epidemiological implications of differing levels of human interaction. We’ve included a portion of the models that we found most powerful:
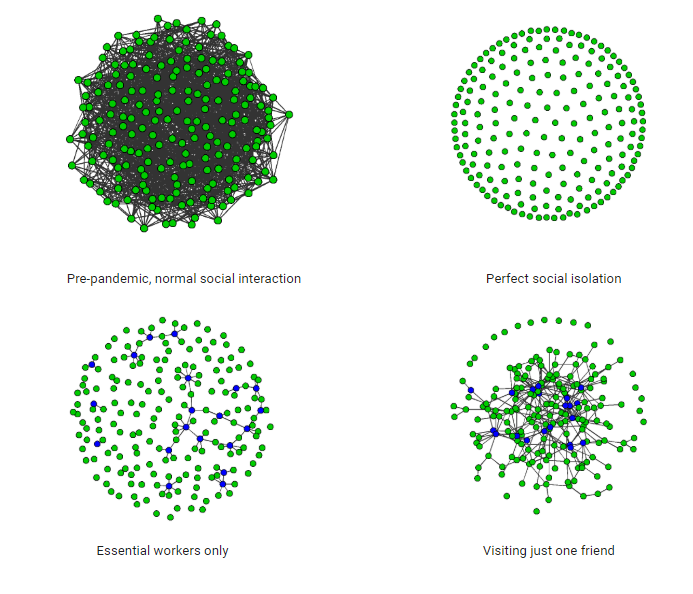
Green dots (nodes) represent individual households. Grey lines represent interactions. Blues nodes represent essential worker households.
We can clearly see the transmission opportunity for infectious diseases, such as Covid-19, positively correlates with social interaction. Simply put, more connections lead to more infections. For the full article from UW please visit http://statnet.org/COVID-JustOneFriend/.
Antibody Testing Update: Are the tests up to the test?
Some 3 billion people in the world are under shelter-in-place orders. As the world’s COVID-19 conversation turns to ‘reopening’ strategy, we wait with droplet-laden breath for serology testing for SARS-CoV-2 antibodies, to help:
- determine who is likely to be protected against re-infection, at least, hopefully, during the time it takes to develop a vaccine and prove it safe and effective.
- measure herd immunity in different populations, since the current models for herd immunity are wide ranging.
- guide return-to-work decisions and duty delegation among healthcare providers.
- verify that vaccines are working as intended in clinical trials.
- identify people who could donate their antibodies for the purpose of injecting them, as potential treatment, into patients with severe COVID-19, or as prevention in people with ongoing high exposure in the healthcare setting (neither is fully proven yet, though we imagine Boris Johnson got some?)
- assess case-fatality rates for COVID-19 in different populations (since ‘recovered’ people who weren’t tested for active disease by PCR in the first place, or had false-negative PCR results, would be added into the denominator).
Leaders sure want serology testing. Gov. Cuomo called on Trump to use the Defense Production Act to help crank out an antibody test that New York has developed on its own – approved by its department of health. Terms like “immunity passports” are being thrown around by even smart people like Dr. Fauci.
Regulators must dance between haste and accuracy. In the US, for example, the FDA in mid-March waved the need for companies to collect accuracy data to usual FDA standards for SARS-CoV-2 antibody testing before going to market. Essentially they are letting companies start selling tests right away once the manufacturer has informed the FDA that the test has been validated internally (notably different from “FDA approval”). By April 7, the FDA reported 70 different antibody test developers having initiated such reporting to them. Many scientists are concerned about this short-cut in accuracy testing, and have leaned on the FDA, CDC, and NIH to perform their own validation of some of these tests on the market (which is likely to occur).
How the heck do antibody tests work anyway? The science is based on the protein(s) on the virus’ coating that triggers a healthy immune system to recognize and neutralize it. Currently, the protein of greatest interest is the so-called viral spike protein. The spike protein is the protein on the viral surface that seems responsible for entry into an infected person’s cells and seems to be the main target for a person’s neutralizing antibodies when fighting COVID-19. One big challenge in creating an antibody test for SARS-CoV-2 is to ‘manufacture’ the spike protein that will be used in testing kits. For example if you engineer a bacteria to produce the spike protein, you hope it doesn’t come out slightly deformed such that the antibodies within the blood of a COVID-19 survivor fail to recognize and bind to it, creating a ‘false negative’ result. Even more concerning, if you engineer the SARS-CoV-2 spike protein for your antibody test in a form that ends up being too similar to the spike protein in one of the four coronaviruses that cause the common cold, you would create some ‘false positive’ results that lead people to feel protected from COVID-19 when they are not. We’re sure there are several other technical and logistical challenges that could be explained to us by a specialized scientist but thank goodness all of them are too busy right now developing antibody testing! Reference for this article: Developing antibody tests for SARS-CoV-2.
Yet another reason to eat your veggies! (We’re always looking for a reason to say that at Wise Patient, right?)
In another example of how everything is connected, coronavirus may shift us all a bit more towards vegetarianism. Several meat processing plants in the US have been sites of COVID-19 outbreaks, and many have been forced to close to protect the safety of their workers. In contrast to other agricultural products we buy at the grocery store, meat requires workers to stand in close proximity in an indoor building while they cut, debone, and package meat, and one plant in South Dakota approximately 10% of the workforce contracted coronavirus before the plant closed. Reference for this article: https://www.nytimes.com/2020/04/13/business/coronavirus-food-supply.html?searchResultPosition=1
Reliable Sources to Stay Updated on the COVID-19 Outbreak
- A comprehensive list of resources is available on our website: https://imwisepatient.com/week-of-3-23-2020/
If you have any questions, please contact our office at: info@wisepatientim.com
